PAH and associated conditions
PAH and Associated Conditions
About connective tissue disease and PAH
Up to 3 in every 20 people with a connective tissue disease (CTD) will go on to develop pulmonary arterial hypertension (PAH). This page has been designed to provide further information and useful resources to help you learn more about CTD-PAH.
On this page you will find information on:
- PAH and the different types of the condition
- The importance of screening for PAH and early diagnosis
- CTD-PAH and its signs and symptoms
- Systemic sclerosis and PAH
- Resources and further information to support you
What is PAH?
- Pulmonary arterial hypertension (PAH) is a rare condition that affects the blood vessels that carry blood from the heart to the lungs. These are known as pulmonary arteries. It is a progressive disease, meaning it can get worse over time.
- With PAH, the pulmonary arteries become increasingly narrow, as the walls of the blood vessels become thicker and less flexible.
- The narrowing of the pulmonary arteries restricts blood flow to the lungs, which makes it harder for the heart to pump blood through the arteries. Trying to maintain the blood flow, the heart has to pump harder, increasing the pressure in the pulmonary arteries.
What does this mean?
- When the right side of the heart has to work continuously harder to pump blood through the pulmonary arteries, it can gradually become weaker. In some cases, this can lead to right heart failure.
- Read our About PAH page for further information on PAH, including symptoms, severity, and how PAH is diagnosed and treated.
There are different sub-types of PAH. This page aims to provide helpful and reliable information to support you in understanding these, by explaining the conditions, their signs and symptoms, as well as their connection to other conditions.
Types of PAH
While there is ongoing research into the cause of PAH, we do know there are four main sub-types.
These include:
Idiopathic PAH

Idiopathic PAH (iPAH) is where there is no obvious cause for PAH. It is the most common sub-type of PAH.
Associated PAH
Associated PAH is when the disease occurs because of the impact of living with other conditions. PAH can be associated with a variety of other conditions including; diseases that affect the tissues holding the body together (also known as connective tissue disease), birth defects that affect the heart (also known as congenital heart disease), HIV and liver disease.

Connective tissue disease (CTD)- PAH
- PAH associated with connective tissue disease (CTD-PAH) is the second most common type of PAH (after idiopathic PAH).
- Because the lungs have lots of connective tissue and blood supply, they can be affected in people living with CTDs.
- PAH can be a complication of CTDs such as systemic sclerosis (SSc), mixed CTD (MCTD), and systemic lupus erythematosus (SLE).
- Further information on CTD-PAH is included below.

Congenital heart disease (CHD)- PAH
- PAH can be a relatively common complication of congenital heart disease (CHD), in fact, PAH is diagnosed in about one in ten people living with CHD.

Portopulmonary hypertension (PoPH)
- Liver disease and portal hypertension (high blood pressure in the vein which carries the blood from the bowel and spleen to the liver) can cause a type of PAH, called portopulmonary hypertension (PoPH). Around 1 in 20 people with advanced liver disease may develop PoPH.
Heritable PAH

Some genes have been found to play a role in the development of PAH and heritable PAH is caused by a problem with a gene that runs in the family. The more that is understood about this genetic link, the more effective treatments for PAH may become.
Drug- and toxin-induced PAH

PAH may develop in people exposed to various drugs and toxins (including drug-related appetite suppressants, beta-interferons, and some tyrosine kinase inhibitors).
Importance of screening and early diagnosis of PAH
What is screening?
If a person is at risk of developing a certain condition, a doctor may carry out tests at regular appointments, even if you are not showing any obvious symptoms, to check the likelihood of the disease developing. Screening is the term used to describe these tests.
Early diagnosis of PAH

Early diagnosis of PAH can be challenging, particularly because the main symptoms, such as breathlessness, dizziness, and tiredness can be confused with more common conditions like asthma and chronic obstructive pulmonary disease (COPD). In some cases, it can take a while to be diagnosed, and because PAH can get worse over time, the symptoms at diagnosis may be more severe and harder to manage with treatment.

Earlier screening can help improve the journey to treatment by reducing the time to a PAH diagnosis and therefore providing the opportunity for the disease to be better managed or for its progression to be slowed.

Learning the signs and symptoms of PAH is important so you know when to speak to your doctor.

For more information about how PAH is diagnosed, click here.
Connective tissue disease and PAH
What is it?
- A connective tissue disease (CTD) is any disease that affects the parts of the body that connect the structures of the body together (e.g. fat, bone, and cartilage).
- Connective tissues are made up of two proteins, which are needed for the body to function properly: collagen and elastin.

Collagen is a protein found in the tendons, ligaments, skin, eyes, bone, and blood vessels.

Elastin is a stretchy protein that resembles a rubber band and is the major component of ligaments and skin.
- When a person has a CTD, the collagen and elastin are inflamed. The proteins and the body parts they connect are harmed.
- Because the lungs have lots of connective tissue and blood supply, they can be particularly affected in people living with CTDs.
Signs and symptoms of CTD-PAH
Because CTDs affect different parts of your body, the symptoms can vary depending on the affected areas. They can include any of a combination of the symptoms below – if you experience any of these symptoms, seek advice from your doctor:
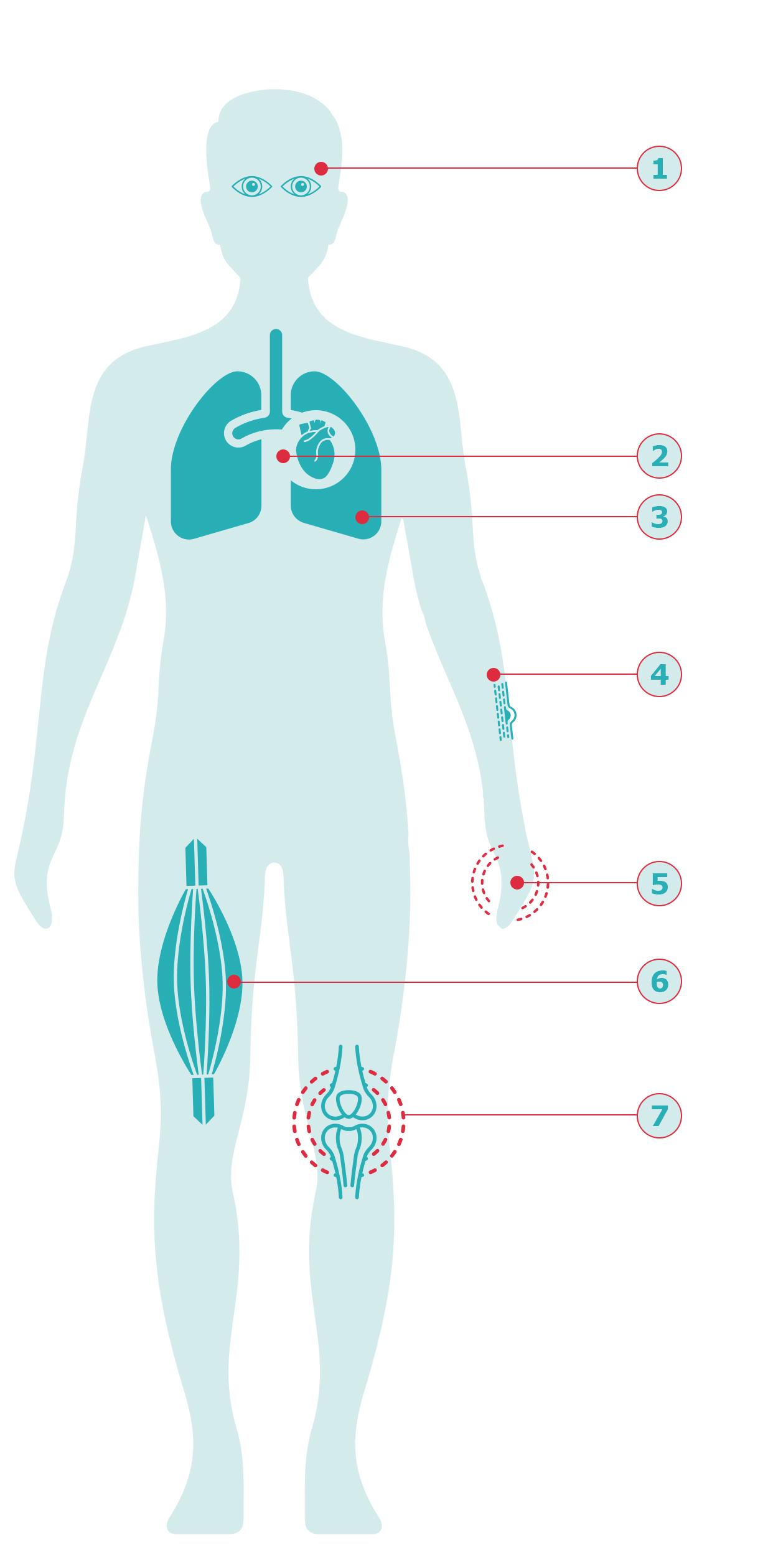
- Changes in sight/vision
- Chest pain
- Breathlessness
- Changes in the skin, such as swelling, colour, or texture (e.g. hardening or thickening)
- Swelling of the fingers
- Muscle weakness
- New or worsening joint pain
Examples of CTDs
There are more than 200 different types of CTD, although those most commonly associated with PAH include:
- Scleroderma:17 Scleroderma means “hard skin” and is a chronic autoimmune condition, meaning it persists for a long time and happens when the body’s own immune system destroys healthy body tissue by mistake. There are two main types of scleroderma:

Localised, affecting just the skin.
Systemic sclerosis (SSc) where blood vessels and internal organs can also be affected. If the heart and lungs are affected by SSc, it can put you at increased risk of developing PAH. You can find out more about SSc and PAH below:

The symptoms of scleroderma can usually be controlled by a range of different treatments, however, while treatments exist, there is currently no cure.18
Also known as lupus, is a disease that can cause inflammation of the connective tissue in every organ of the body, from the brain, skin, blood, to the lungs.1819 While numbers vary, it is estimated that about one in 12 people with SLE may develop PAH, and it is nine times more common in women than in men.2021

A condition that has some, but not all, features of various connective tissue diseases, such as SLE, scleroderma, and other CTDs. When features of these different conditions overlap, doctors may diagnose it as MCTD.22 About one in 12 people with PAH also has MCTD.23
If you have been diagnosed with SLE or MCTD, make sure you speak with your doctor if you have any concerns about PAH, or are showing symptoms as highlighted above. They will be able to support you in providing guidance and carry out the appropriate tests. If you have SSc, you can find further information on SSc-PAH below.
Systemic sclerosis and PAH
Systemic sclerosis (SSc) and PAH accounts for 74% of all CTD-PAH diagnoses.23 This section includes further information to help you learn more about SSc-PAH.
SSc-PAH
- About 3 in every 25 people with SSc go on to develop PAH, and SSc-PAH accounts for 74% of all CTD-PAH diagnoses.2324
- Although there is currently no available cure, there are treatments available that can help people with SSc-PAH to better manage their symptoms, and there are number of ongoing research studies into new medicines for the disease.25
Signs and symptoms of SSc-PAH
- People with SSc-PAH may experience difficulty breathing that gets worse over time, tiredness, or chest palpitations but often they are unaware these symptoms are connected to PAH.26
- In people with SSc, if any of the following symptoms occur, it’s important to seek advice from a doctor as soon as possible: shortness of breath, light-headedness, swelling in the feet or ankles, and chest pain.26
Speaking with your doctor about SSc-PAH
.png?width=625&height=556&format=png&quality=50)
- If you are living with SSc, you may want to speak to your doctor about being screened for PAH each year. Screening is the term used to describe the tests a doctor may carry out if a person is at risk of developing a certain condition, even if you are not showing obvious symptoms.
- It has been shown that finding SSc-PAH early, through screening people with SSc, can slow the progression of PAH.
- Recording your symptoms as well as how and when they started, and sharing this information with your doctor can help them decide when and how best to test for PAH – remember some symptoms are subtle and may not be obvious but it can be helpful to record all your experiences and discuss them with your doctor.
- If you, or a loved one are thinking about having a baby, it’s important that you speak with your doctor, given there are some extra risks with pregnancy if you have CTD-PAH. The majority of pregnancies in people with CTD-PAH do go to plan, however your doctor will want to carry out the appropriate tests throughout your pregnancy and support you with creating a plan of care.27
