What is PAH?
What is PAH?
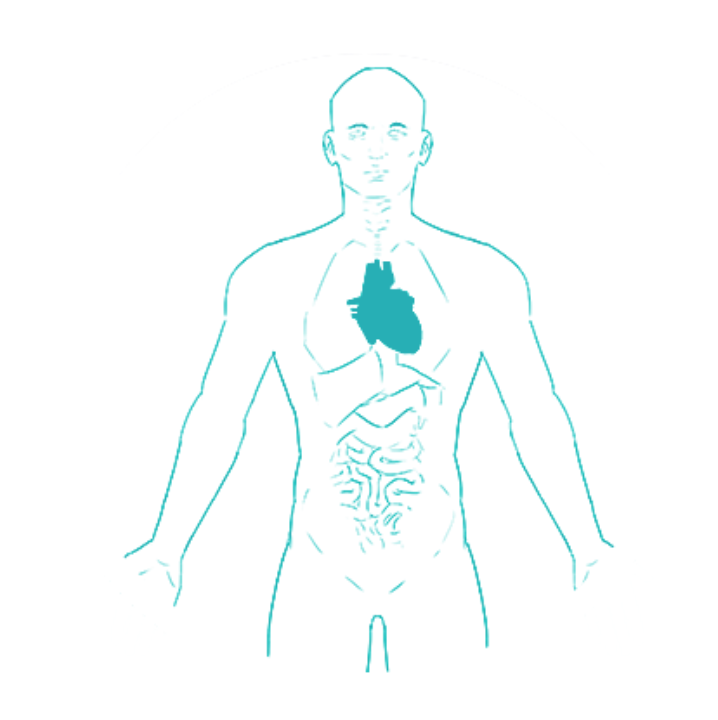
Pulmonary arterial hypertension (PAH) is a rare condition that affects the blood vessels that carry blood from the heart to the lungs. These are known as pulmonary arteries. It is a progressive disease, meaning it can get worse over time.
With PAH, the pulmonary arteries become increasingly narrow, as the walls of the blood vessels become thicker and less flexible. The narrowing of the pulmonary arteries restricts blood flow to the lungs, which makes it harder for the heart to pump blood through the arteries. Trying to maintain the blood flow, the heart has to pump harder, increasing the pressure in the pulmonary arteries.
What does this mean?
When the right side of the heart has to work continuously harder to pump blood through the pulmonary arteries, it can gradually become weaker. In some cases, this can lead to right heart failure.
Watch the What is PAH video to find out more
What are the symptoms of PAH?

Breathlessness is often the first symptom of PAH. It is often noticed when undertaking physical activities, such as climbing up stairs or running. As PAH progresses, other signs and symptoms may develop and affect everyday activities.
Symptoms may include:
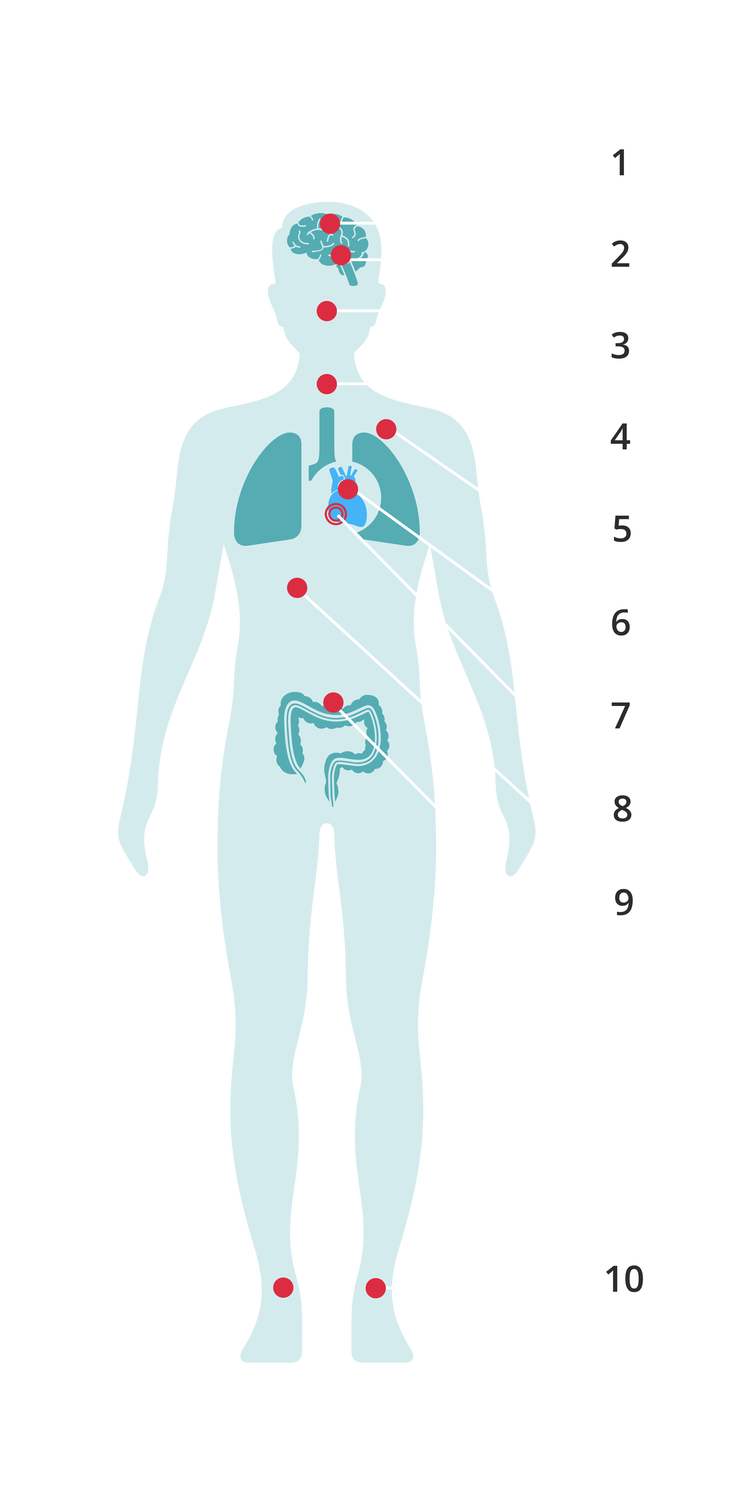
2. Dizziness
3. Breathing difficulty
4. Cough
5. Chest pain
6. Heart failure
7. Arrhythmias (abnormality of the heart's rhythm)
8. Fatigue
9. Ascites (build up of fluid in the abdomen)
10. Oedema (swelling)
What causes PAH?

We still do not fully understand PAH and an exact cause is unknown. However, there are four main kinds of PAH. These include:

Idiopathic PAH is where there is no obvious cause for PAH. It is the most common type of PAH.

Heritable PAH is caused by a problem with a gene that runs in the family. The more that is understood about this genetic link, the more effective treatments for PAH may become.

Associated PAH is when the disease occurs because of the impact of living with other conditions. PAH can be associated with a variety of other conditions including; diseases that affect the tissues holding the body together (also known as connective tissue disease), birth defects that affect the heart (also known as congenital heart disease), HIV and liver disease.
For more information about PAH and its associated conditions, visit the PAH and Associated Conditions page
Drug and toxin induced PAH is where certain drugs and toxins can bring about PAH.
How is PAH diagnosed?

Early diagnosis of PAH is important as it is linked with better health outcomes, however, PAH is often difficult to diagnose. A key problem is that the early symptoms - breathlessness, dizziness and fatigue - are not very specific and can be easily confused with many other, more common conditions like asthma or even lack of fitness or depression. Due to its complexity, PAH is usually diagnosed at specialist centres where healthcare professionals (HCPs) conduct a series of tests to rule out other possible conditions, and confirm diagnosis.
Tests available to suspect and confirm a PAH diagnosis include:

Clinical examination

Electrocardiogram (ECG)
A simple test that measures your heart’s electrical activity

Chest radiograph
A chest X-ray to create a picture of the structures in and around the chest
Pulmonary function tests (PFTs) and arterial blood gases
Breathing tests that show how well the lungs are working by measuring lung volume, capacity, rate of gas flow, and gas exchange

Echocardiography
An ultrasound scan used to look at the heart and nearby blood vessels
Ventilation/Perfusion scan (V/Q scan)
A scan to examine airflow (ventilation) and blood flow (perfusion) in the lungs
High-resolution computed tomography (CT scan), contrast-enhanced computed tomography, and pulmonary angiography
A CT imaging scan can provide important information on vascular, cardiac, parenchymal and mediastinal abnormalities
Cardiac magnetic resonance imaging
An imaging test (also known as a cMRI) to create comprehensive pictures of the heart
Blood tests and immunology
Important measures include testing for N-terminal pro-brain natriuretic peptide (NT-proBNP) as this may be elevated in patients with PH

Cardiopulmonary exercise testing (CPET)
A specific type of stress test that measures your exercise ability

Abdominal ultrasound scan
A procedure that uses sound waves to look and create an image inside the body

Right heart catheterisation and vasoreactivity test
An invasive procedure that enables direct and accurate measurement of the condition of the right heart and pulmonary vessels. This is the definitive test for diagnosing PAH
Genetic testing
Trained professionals can test for specific gene mutations including the BMPR2 mutation. Genetic counselling should also be offered
How is PAH treated?

There are several specific medicines to treat PAH. All listed medicines relax and widen the blood vessels in the lungs as well as reduce and prevent the overgrowth of cells in the walls of the vessels. To help people with PAH get the best quality of life possible, PAH specialists may recommend one or more treatments including oral, inhaled and intravenous medications, at a time. In severe cases, lung transplantation may be needed.
Other supportive treatments that may be recommended for PAH include:
- Blood thinners to prevent clots
- Diuretics (also called water tablets) to reduce swelling
- Supplementary oxygen to ensure the body has enough to function
- Iron supplementation, as iron deficiency can be common in people with PAH
- Physical activity and supervised rehabilitation
- Psychological support
People living with PAH are advised to speak to their HCP to identify the best treatment option for them. While there is no cure for PAH yet, treatments can help people manage and slow progression of the condition.
Progression of PAH

A progressive condition is a disease that, in most cases, worsens over time.
In PAH the term ‘functional class’ is commonly used to assess the severity of the disease and can be used to evaluate the progression of the condition and to determine treatments. PAH is categorised into four functional classes:
Functional Class I – Patients with pulmonary hypertension but without resulting limitation of physical activity. Ordinary physical activity does not cause undue dyspnoea or fatigue, chest pain or near syncope.
Functional Class II – Patients with pulmonary hypertension resulting in slight limitation of physical activity. They are comfortable at rest. Ordinary physical activity causes undue dyspnoea or fatigue, chest pain or near syncope.
Functional Class III – Patients with pulmonary hypertension resulting in marked limitation of physical activity. They are comfortable at rest. Less than ordinary activity causes undue dyspnoea or fatigue, chest pain or near syncope.
Functional Class IV – Patients with pulmonary hypertension with inability to carry out any physical activity without symptoms. These patients manifest signs of right heart failure. Dyspnoea and/or fatigue may even be present at rest. Discomfort is increased by any physical activity.
Table from ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension
In current management of PAH, the risk of disease progression in patients is assessed with a comprehensive set of clinical tests, imaging and biomarkers, rather than just WHO functional class. It is important to perform this risk assessment regularly over the course of your disease to identify early signs of disease progression and escalate treatment as appropriate.
Visit the Living Well with PAH page or Useful links and tools page for more information.
